1.The definition of Pain
Pain is a distressing feeling often caused by intense or damaging stimuli. The International Association for the Study of Pain defines pain as “an unpleasant sensory and emotional experience associated with, or resembling that associated with, actual or potential tissue damage.”[1-2] In medical diagnosis, pain is regarded as a symptom of an underlying condition.
Pain motivates the individual to withdraw from damaging situations, to protect a damaged body part while it heals, and to avoid similar experiences in the future.[2] Most pain resolves once the noxious stimulus is removed and the body has healed, but it may persist despite removal of the stimulus and apparent healing of the body. Sometimes pain arises in the absence of any detectable stimulus, damage or disease.[3]
Pain is the most common reason for physician consultation in most developed countries.[4-5] It is a major symptom in many medical conditions, and can interfere with a person’s quality of life and general functioning.[6]
Classification
The International Association for the Study of Pain recommends using specific features to describe a patient’s pain:
- region of the body involved (e.g. abdomen, lower limbs),
- system whose dysfunction may be causing the pain (e.g., nervous, gastrointestinal),
- duration and pattern of occurrence,
- intensity, and
- cause[6]
Reference:
[1]The revised International Association for the Study of Pain definition of pain: concepts, challenges, and compromises.
[2]Understanding Pain : Exploring the Perception of Pain.
[4]Caring for patients with chronic pain: pearls and pitfalls.
[5]What should be the core outcomes in chronic pain clinical trials?
[6]Classification of Chronic Pain.
2.Pain theories*
2.1 Historical
Before the relatively recent discovery of neurons and their role in pain, various different body functions were proposed to account for pain. There were several competing early theories of pain among the ancient Greeks: Hippocrates believed that it was due to an imbalance in vital fluids.[1] In the 11th century, Avicenna theorized that there were a number of feeling senses including touch, pain and titillation.[2]
In 1644, René Descartes theorized that pain was a disturbance that passed down along nerve fibers until the disturbance reached the brain.[3-4] Descartes’s work, along with Avicenna’s, prefigured the 19th-century development of specificity theory. Specificity theory saw pain as “a specific sensation, with its own sensory apparatus independent of touch and other senses”.[5] Another theory that came to prominence in the 18th and 19th centuries was intensive theory, which conceived of pain not as a unique sensory modality, but an emotional state produced by stronger than normal stimuli such as intense light, pressure or temperature.[6] By the mid-1890s, specificity was backed mostly by physiologists and physicians, and the intensive theory was mostly backed by psychologists. However, after a series of clinical observations by Henry Head and experiments by Max von Frey, the psychologists migrated to specificity almost en masse, and by century’s end, most textbooks on physiology and psychology were presenting pain specificity as fact.[2,5]
2.2 Modern
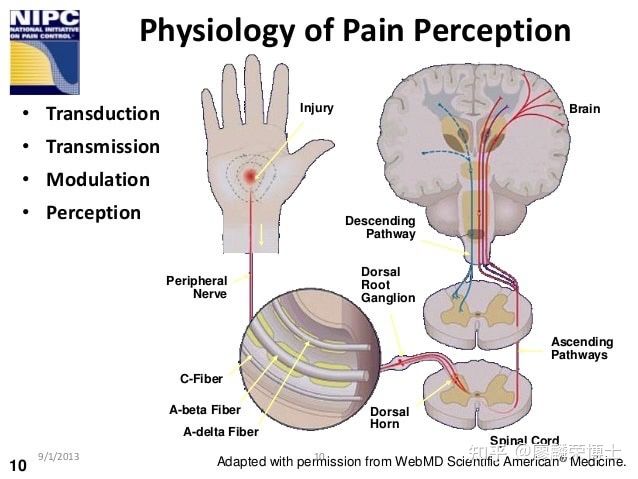
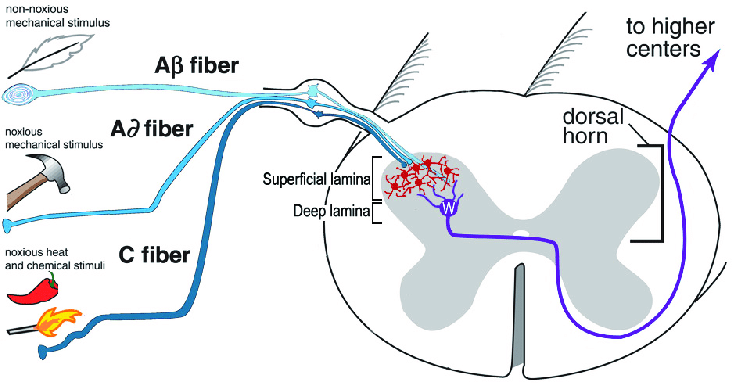
Some sensory fibers do not differentiate between noxious and non-noxious stimuli, while others, nociceptors, respond only to noxious, high intensity stimuli. At the peripheral end of the nociceptor, noxious stimuli generate currents that, above a given threshold, send signals along the nerve fiber to the spinal cord. The “specificity” (whether it responds to thermal, chemical or mechanical features of its environment) of a nociceptor is determined by which ion channels it expresses at its peripheral end. Dozens of different types of nociceptor ion channels have so far been identified, and their exact functions are still being determined.[7]
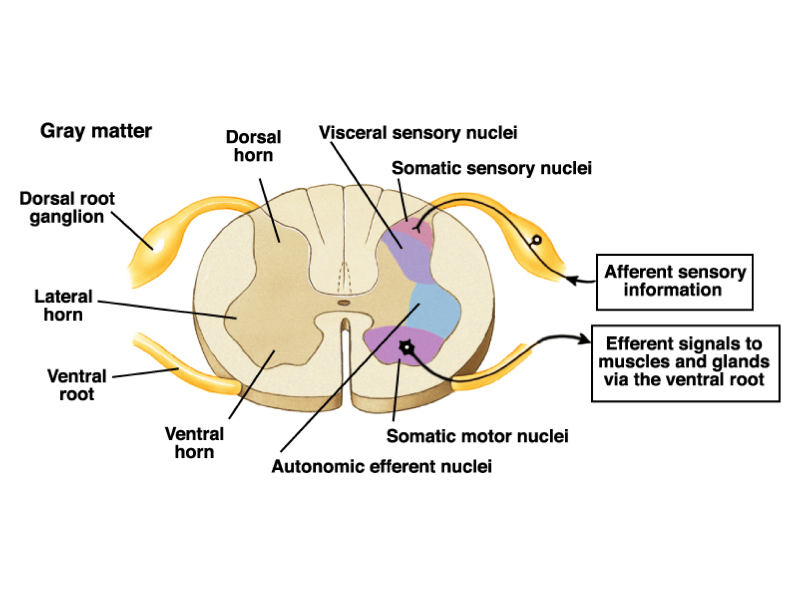
The pain signal travels from the periphery to the spinal cord along an A-delta or C fiber. Because the A-delta fiber is thicker than the C fiber, and is thinly sheathed in an electrically insulating material (myelin), it carries its signal faster (5–30 m/s) than the unmyelinated C fiber (0.5–2 m/s).[8]Pain evoked by the A-delta fibers is described as sharp and is felt first. This is followed by a duller pain, often described as burning, carried by the C fibers.[9] These A-delta and C fibers enter the spinal cord via Lissauer’s tract and connect with spinal cord nerve fibers in the central gelatinous substance of the spinal cord. These spinal cord fibers then cross the cord via the anterior white commissure and ascend in the spinothalamic tract. Before reaching the brain, the spinothalamic tract splits into the lateral, neospinothalamic tract and the medial, paleospinothalamic tract. The neospinothalamic tract carries the fast, sharp A-delta signal to the ventral posterolateral nucleus of the thalamus. The paleospinothalamic tract carries the slow, dull, C-fiber pain signal. Some of these fibers peel off in the brain stem, connecting with the reticular formation or midbrain periaqueductal gray, and the remainder terminate in the intralaminar nuclei of the thalamus.[9]
Pain-related activity in the thalamus spreads to the insular cortex (thought to embody, among other things, the feeling that distinguishes pain from other homeostatic emotions such as itch and nausea) and anterior cingulate cortex (thought to embody, among other things, the affective/motivational element, the unpleasantness of pain),[10] and pain that is distinctly located also activates primary and secondary somatosensory cortex.[11]
Spinal cord fibers dedicated to carrying A-delta fiber pain signals, and others that carry both A-delta and C fiber pain signals to the thalamus have been identified. Other spinal cord fibers, known as wide dynamic range neurons, respond to A-delta and C fibers, but also to the large A-beta fibers that carry touch, pressure and vibration signals.[8] In 1955, DC Sinclair and G Weddell developed peripheral pattern theory, based on a 1934 suggestion by John Paul Nafe. They proposed that all skin fiber endings (with the exception of those innervating hair cells) are identical, and that pain is produced by intense stimulation of these fibers.[5] Another 20th-century theory was gate control theory, introduced by Ronald Melzack and Patrick Wall in the 1965 Science article “Pain Mechanisms: A New Theory”.[12] The authors proposed that both thin (pain) and large diameter (touch, pressure, vibration) nerve fibers carry information from the site of injury to two destinations in the dorsal horn of the spinal cord, and that the more large fiber activity relative to thin fiber activity at the inhibitory cell, the less pain is felt.[13]
Three dimensions of pain
In 1968 Ronald Melzack and Kenneth Casey described chronic pain in terms of its three dimensions:
- “sensory-discriminative” (sense of the intensity, location, quality and duration of the pain),
- “affective-motivational” (unpleasantness and urge to escape the unpleasantness), and
- “cognitive-evaluative” (cognitions such as appraisal, cultural values, distraction and hypnotic suggestion).
They theorized that pain intensity (the sensory discriminative dimension) and unpleasantness (the affective-motivational dimension) are not simply determined by the magnitude of the painful stimulus, but “higher” cognitive activities can influence perceived intensity and unpleasantness.Thus, excitement in games or war appears to block both the sensory-discriminative and affective-motivational dimensions of pain, while suggestion and placebos may modulate only the affective-motivational dimension and leave the sensory-discriminative dimension relatively undisturbed.The paper ends with a call to action: “Pain can be treated not only by trying to cut down the sensory input by anesthetic block, surgical intervention and the like, but also by influencing the motivational-affective and cognitive factors as well.”
Reference:
[1]Models of Pain Perception.
[2]Pain: History and present status.
[3]Models of Pain Perception.
[4]The Gate Control Theory: Reaching for the Brain.
[5]History of pain concepts and therapies.
[6]Origins of neuroscience: a history of explorations into brain function.
[7]Nociceptors—noxious stimulus detectors.
[8]Applied pain neurophysiology.
[9]Psychology of pain.
[10]Pain mechanisms: labeled lines versus convergence in central processing.
[11]The functional anatomy of neuropathic pain.
[12]Pain mechanisms: a new theory.
[13]The Gate Control Theory: Reaching for the Brain.
3.Mechanisms of pain
3.1 Nociceptive pain
Nociceptive pain is caused by stimulation of sensory nerve fibers that respond to stimuli approaching or exceeding harmful intensity (nociceptors), and may be classified according to the mode of noxious stimulation. The most common categories are “thermal” (e.g. heat or cold), “mechanical” (e.g. crushing, tearing, shearing, etc.) and “chemical” (e.g. iodine in a cut or chemicals released during inflammation). Some nociceptors respond to more than one of these modalities and are consequently designated polymodal.
Nociceptive pain may also be classed according to the site of origin and divided into “visceral”, “deep somatic” and “superficial somatic” pain. Visceral structures (e.g., the heart, liver and intestines) are highly sensitive to stretch, ischemia and inflammation, but relatively insensitive to other stimuli that normally evoke pain in other structures, such as burning and cutting. Visceral pain is diffuse, difficult to locate and often referred to a distant, usually superficial, structure. It may be accompanied by nausea and vomiting and may be described as sickening, deep, squeezing, and dull.[1] Deep somatic pain is initiated by stimulation of nociceptors in ligaments, tendons, bones, blood vessels, fasciae and muscles, and is dull, aching, poorly-localized pain. Examples include sprains and broken bones. Superficial somatic pain is initiated by activation of nociceptors in the skin or other superficial tissue, and is sharp, well-defined and clearly located. Examples of injuries that produce superficial somatic pain include minor wounds and minor (first degree) burns.[2]
3.1.1 Noxious stimulus
3.1.2 Nociception
3.2 Neuropathic pain
Neuropathic pain is caused by damage or disease affecting any part of the nervous system involved in bodily feelings (the somatosensory system).[1] Neuropathic pain may be divided into peripheral, central, or mixed (peripheral and central) neuropathic pain. Peripheral neuropathic pain is often described as “burning”, “tingling”, “electrical”, “stabbing”, or “pins and needles”.[2] Bumping the “funny bone” elicits acute peripheral neuropathic pain.
Some manifestations of neuropathic pain include: traumatic neuropathy, tic douloureux, painful diabetic neuropathy, and postherpetic neuralgia.[3]
Reference:
[1]Neuropathic pain: redefinition and a grading system for clinical and research purposes.
[2]Mechanisms and management of neuropathic pain in cancer.
[3]Mechanisms of neuropathic pain.
3.3 Nociplastic pain
Nociplastic pain is pain characterized by a changed nociception (but without evidence of real or threatened tissue damage, or without disease or damage in the somatosensory system).[1] In some debates regarding physician-assisted suicide or euthanasia, pain has been used as an argument to permit people who are terminally ill to end their lives.[2] This applies, for example, to fibromyalgia patients.
Reference:
[1]Mind-Body Therapies for Opioid-Treated Pain: A Systematic Review and Meta-analysis.
[2]Explaining the emergence of euthanasia law in the Netherlands: how the sociology of law can help the sociology of bioethics.
3.4 Psychogenic pain
Psychogenic pain, also called psychalgia or somatoform pain, is pain caused, increased or prolonged by mental, emotional or behavioral factors.[1] Headache, back pain and stomach pain are sometimes diagnosed as psychogenic.[1] Sufferers are often stigmatized, because both medical professionals and the general public tend to think that pain from a psychological source is not “real”. However, specialists consider that it is no less actual or hurtful than pain from any other source.[2]
People with long-term pain frequently display psychological disturbance, with elevated scores on the Minnesota Multiphasic Personality Inventory scales of hysteria, depression and hypochondriasis (the “neurotic triad”). Some investigators have argued that it is this neuroticism that causes acute pain to turn chronic, but clinical evidence points the other direction, to chronic pain causing neuroticism. When long-term pain is relieved by therapeutic intervention, scores on the neurotic triad and anxiety fall, often to normal levels. Self-esteem, often low in chronic pain patients, also shows improvement once pain has resolved.[3]
Reference:
[1]Psychogenic Pain.
[2]International Association for the Study of Pain Pain Definitions. [3]The challenge of pain.
4.Somatosensory system
4.1 Sensory nervous system*
4.2 sensory nerve fibers
4.3 Nociceptor
4.4 Dorsal root ganglion
5.Evolutionary and behavioral role of pain
Pain is part of the body’s defense system, producing a reflexive retraction from the painful stimulus, and tendencies to protect the affected body part while it heals, and avoid that harmful situation in the future.[1-2] It is an important part of animal life, vital to healthy survival. People with congenital insensitivity to pain have reduced life expectancy.[3]
In The Greatest Show on Earth: The Evidence for Evolution, biologist Richard Dawkins addresses the question of why pain should have the quality of being painful. He describes the alternative as a mental raising of a “red flag”. To argue why that red flag might be insufficient, Dawkins argues that drives must compete with one other within living beings. The most “fit” creature would be the one whose pains are well balanced. Those pains which mean certain death when ignored will become the most powerfully felt. The relative intensities of pain, then, may resemble the relative importance of that risk to our ancestors (For example, lack of food, extreme cold, or serious injuries are felt as exceptionally painful, whereas minor damage is felt as mere discomfort). This resemblance will not be perfect, however, because natural selection can be a poor designer. This may have maladaptive results such as supernormal stimuli.[4]
Pain, however, does not only wave a “red flag” within living beings but may also act as a warning sign and a call for help to other living beings. Especially in humans who readily helped each other in case of sickness or injury throughout their evolutionary history, pain might be shaped by natural selection to be a credible and convincing signal of need for relief, help, and care.[5]
Idiopathic pain (pain that persists after the trauma or pathology has healed, or that arises without any apparent cause) may be an exception to the idea that pain is helpful to survival, although some psychodynamic psychologists argue that such pain is psychogenic, enlisted as a protective distraction to keep dangerous emotions unconscious.[6]
Reference:
[1]Cutaneous nociceptors.
[2]The neuroevolution of motivation.
[3]Congenital insensitivity to pain: an update.
[4]The Greatest Show on Earth.
[5]An Evolutionary Perspective on Pain Communication.
[6]The divided mind: the epidemic of mindbody disorders.
6.Threshold of pain
In pain science, thresholds are measured by gradually increasing the intensity of a stimulus in a procedure called quantitative sensory testing which involves such stimuli as electric current, thermal (heat or cold), mechanical (pressure, touch, vibration), ischemic, or chemical stimuli applied to the subject to evoke a response.[1] The “pain perception threshold” is the point at which the subject begins to feel pain, and the “pain threshold intensity” is the stimulus intensity at which the stimulus begins to hurt. The “pain tolerance threshold” is reached when the subject acts to stop the pain.[1]
6.1 pain perception threshold
6.2 pain tolerance threshold
Reference:
[1]Assessment of Chronic Pain: Domains, Methods, and Mechanisms.
7.Allodynia
Allodynia is pain experienced in response to a normally painless stimulus.[1] It has no biological function and is classified by stimuli into dynamic mechanical, punctate and static.[1][2]
Reference:
[1]Allodynia and hyperalgesia in neuropathic pain: clinical manifestations and mechanisms.
[2]Mechanical allodynia.
8.Pain asymbolia
Although unpleasantness is an essential part of the IASP definition of pain,[1] it is possible to induce a state described as intense pain devoid of unpleasantness in some patients, with morphine injection or psychosurgery. Such patients report that they have pain but are not bothered by it; they recognize the sensation of pain but suffer little, or not at all.[2] Indifference to pain can also rarely be present from birth; these people have normal nerves on medical investigations, and find pain unpleasant, but do not avoid repetition of the pain stimulus.[3]
Reference:
[1]International Association for the Study of Pain: Pain Definitions.
[2]Feeling pain and being in pain.
[3]Congenital insensitivity to pain: an update.
9.Congenital insensitivity to pain
Insensitivity to pain may also result from abnormalities in the nervous system. This is usually the result of acquired damage to the nerves, such as spinal cord injury, diabetes mellitus (diabetic neuropathy), or leprosy in countries where that disease is prevalent.[1] These individuals are at risk of tissue damage and infection due to undiscovered injuries.
A much smaller number of people are insensitive to pain due to an inborn abnormality of the nervous system, known as “congenital insensitivity to pain”.[2] Children with this condition incur carelessly-repeated damage to their tongues, eyes, joints, skin, and muscles. Some die before adulthood, and others have a reduced life expectancy. Most people with congenital insensitivity to pain have one of five hereditary sensory and autonomic neuropathies (which includes familial dysautonomia and congenital insensitivity to pain with anhidrosis).[3] These conditions feature decreased sensitivity to pain together with other neurological abnormalities, particularly of the autonomic nervous system.[2-3] A very rare syndrome with isolated congenital insensitivity to pain has been linked with mutations in the SCN9A gene, which codes for a sodium channel (Nav1.7) necessary in conducting pain nerve stimuli.[4]
Reference:
[1]The gift of pain: why we hurt & what we can do about it.
[2]Congenital insensitivity to pain: an update.
[3]Inherited autonomic neuropathies.
[4]Pain as a channelopathy.
10.Functional effects of pain
Experimental subjects challenged by acute pain and patients in chronic pain experience impairments in attention control, working memory, mental flexibility, problem solving, and information processing speed.[1] Acute and chronic pain are also associated with increased depression, anxiety, fear, and anger.[2]
Reference:
[1]Cognitive impairment in patients with chronic pain: the significance of stress.
[2]Pain-related effects of trait anger expression: neural substrates and the role of endogenous opioid mechanisms.
[3]Inherited autonomic neuropathies.
[4]Pain as a channelopathy.
11.Pain assessment
A person’s self-report is the most reliable measure of pain.[1-3] Some health care professionals may underestimate pain severity.[4] A definition of pain widely employed in nursing, emphasizing its subjective nature and the importance of believing patient reports, was introduced by Margo McCaffery in 1968: “Pain is whatever the experiencing person says it is, existing whenever he says it does”.[5] To assess intensity, the patient may be asked to locate their pain on a scale of 0 to 10, with 0 being no pain at all, and 10 the worst pain they have ever felt. Quality can be established by having the patient complete the McGill Pain Questionnaire indicating which words best describe their pain.[6]
Reference:
[1]Health & physical assessment in nursing.
[2]Fundamentals of nursing : the art and science of person-centered nursing care.
[3]Taber’s cyclopedic medical dictionary.
[4] Underestimation of pain by health-care providers: towards a model of the process of inferring pain in others.
[5]Nursing practice theories related to cognition, bodily pain, and man-environment interactions.
[6]Assessment of pain.
12.Visual analogue scale
The visual analogue scale is a common, reproducible tool in the assessment of pain and pain relief.[1] The scale is a continuous line anchored by verbal descriptors, one for each extreme of pain where a higher score indicates greater pain intensity. It is usually 10 cm in length with no intermediate descriptors as to avoid marking of scores around a preferred numeric value. When applied as a pain descriptor, these anchors are often ‘no pain’ and ‘worst imaginable pain”. Cut-offs for pain classification have been recommended as no pain (0-4mm), mild pain (5-44mm), moderate pain (45-74mm) and severe pain (75-100mm).[2]
Reference:
[1]The minimum clinically significant difference in visual analogue scale pain score does not differ with severity of pain.
[2]Measures of adult pain: Visual Analog Scale for Pain (VAS Pain), Numeric Rating Scale for Pain (NRS Pain), McGill Pain Questionnaire (MPQ), Short-Form McGill Pain Questionnaire (SF-MPQ), Chronic Pain Grade Scale (CPGS), Short Form-36 Bodily Pain Scale (SF-36 BPS), and Measure of Intermittent and Constant Osteoarthritis Pain (ICOAP).
13.Quantitative sensory testing
Integrate static (pain threshold, tolerance, suprathreshold) and dynamic (conditioned pain modulation, offset analgesia, temporal summation) pain reactivity measure.[1]
Quantitative sensory testing (QST) is a rapidly expanding pain research domain that involves measuring psychophysiological responses to standardized experimental stimuli. QST has numerous clinical and research applications (e.g., assessing pain pathophysiology, analgesic evaluation). Static QST measures assess fixed nervous system states, whereas dynamic measures activate and evaluate complex nervous system processes.[1]
Reference:
[1]De Vita, M. J., et al. (2021). “Development of a novel brief quantitative sensory testing protocol that integrates static and dynamic pain assessments: Test-retest performance in healthy adults.” Pain Med.
14.Other reporting barriers
The way in which one experiences and responds to pain is related to sociocultural characteristics, such as gender, ethnicity, and age.[1-2] An aging adult may not respond to pain in the same way that a younger person might. Their ability to recognize pain may be blunted by illness or the use of medication. Depression may also keep older adult from reporting they are in pain. Decline in self-care may also indicate the older adult is experiencing pain. They may be reluctant to report pain because they do not want to be perceived as weak, or may feel it is impolite or shameful to complain, or they may feel the pain is a form of deserved punishment.[3-4]
Cultural barriers may also affect the likelihood of reporting pain. Sufferers may feel that certain treatments go against their religious beliefs. They may not report pain because they feel it is a sign that death is near. Many people fear the stigma of addiction, and avoid pain treatment so as not to be prescribed potentially addicting drugs. Many Asians do not want to lose respect in society by admitting they are in pain and need help, believing the pain should be borne in silence, while other cultures feel they should report pain immediately to receive immediate relief.[5]
Gender can also be a perceived factor in reporting pain. Gender differences can be the result of social and cultural expectations, with women expected to be more emotional and show pain, and men more stoic.[5] As a result, female pain is often stigmatized, leading to less urgent treatment of women based on social expectations of their ability to accurately report it.[6] This leads to extended emergency room wait times for women and frequent dismissal of their ability to accurately report pain.[7-8]
Reference:
[1]Social science and the study of pain since Zborowski: a need for a new agenda.
[2]People in Pain.
[3]Social Construction of pain and aging: Individual artfulness within interpretive structures.
[4]Chronic Pain Management in the Long Term Care Setting: Clinical Practice Guidelines.
[5]Physical examination & health assessment.
[6]When Doctors Don’t Listen to Women.
[7]How Doctors Take Women’s Pain Less Seriously.
[8]Stories of Misunderstanding Women’s Pain.
15.Physiological measurement
Functional magnetic resonance imaging brain scanning (fMRI) has been used to measure pain, and correlates well with self-reported pain.
16.大脑对疼痛的调节
17.疼痛生理学:temporal summation与wind-up现象
wind-up是指脊髓中二级神经元的放电逐渐增加,以响应重复的C纤维刺激,在人类中表现为疼痛增加;wind-up是该过程的一部分,称为中枢敏化。
Temporal summation of pain (i.e. increasing pain perception to repetitive stimulation at the same intensity) is the perceptual correlate in humans that is thought to mimic the early phase of the wind-up process in dorsal horn neurons (Arendt-Nielsen, 1997).[1]
Reference:
[1]Nie, H., et al. (2009). “Temporal summation of pressure pain during muscle hyperalgesia evoked by nerve growth factor and eccentric contractions.” Eur J Pain 13(7): 704-710.
18.神经病理性疼痛
神经病理性疼痛可能与感觉障碍(定义为不愉快的异常感觉)、痛觉超敏(allodynia,一种对于非有害刺激的感觉疼痛,如轻触)和痛觉过敏有关(hyperalgesia, 对正常有害刺激的反应增强)。冷痛觉过敏更是周围神经损伤引起的神经病理性疼痛的一个共同特征。在神经病理性疼痛患者身上观察到的其他规律性特征是:疼痛的时间总和异常,刺激停止后疼痛持续。
19.疼痛研究的项目申请:Influence of Genetics in Pain Sensitivity
Influence of Genetics in Pain Sensitivity
The purpose of this study is to learn more about the role of genetics in pain sensitivity. Pain perception varies widely among individuals, and information gained from this trial may lead to better methods of preventing and controlling pain.
Variability in pain sensitivity is a well known phenomena. Clinicians involved in the care of post-surgical patients are very familiar with this variation in sensitivity. The variability also extends to experimental pain stimuli (e.g., a thermal pulse to the forearm) and can be demonstrated with normal volunteers. In our clinic, variation in the intensity and onset of acute pain in the oral surgery model, in subjects matched for similar levels of tissue injury ranges from little or no post-operative pain to reports of severe pain unrelieved by standard analgesics. While a variety of factors may account for the variability such as race or gender (Gordon 1998), preclinical data indicate that genetic factors profoundly influence pain sensitivity. Thus, the proposed study seeks to investigate genetic contributions to acute experimental and clinical post-operative pain. We have recently shown a strong correspondence between pain reports using thermal heat stimuli and post-operative pain reports. This observation has given us an important quantitative screening tool for genetic analysis of a moderate-sized cohort of subjects that has direct clinical relevance. Normal subjects and their siblings and/or parents will undergo two somatosensory tests to determine pain phenotype and will provide a blood sample which will be analyzed for genetic polymorphisms contributing to sensitivity to pain. Some of these subjects will also be candidates for the oral surgery protocol and similar pain ratings will be obtained from them post-operatively. The initial study will examine known polymorphisms for candidate genes that code for pain sensing and pain suppressing molecules.
20.Why do some people hurt more than others?
Anyone who came of age in the 1990s remembers the “Friends” episode where Phoebe and Rachel venture out to get tattoos. Spoiler alert: Rachel gets a tattoo and Phoebe ends up with a black ink dot because she couldn’t take the pain. This sitcom storyline is funny, but it also simply illustrates the question that I and many others in the field of “pain genetics” are trying to answer. What is it about Rachel that makes her different from Phoebe? And, more importantly, can we harness this difference to help the “Phoebes” of the world suffer less by making them more like the “Rachels”?
Pain is the single most common symptom reported when seeking medical attention. Under normal circumstances, pain signals injury, and the natural response is to protect ourselves until we have recovered and the pain subsides. Unfortunately, people differ not only in their ability to detect, tolerate and respond to pain but also in how they report it and how they respond to various treatments. This makes it difficult to know how to effectively treat each patient. So, why isn’t pain the same in everyone?
Individual differences in health outcomes often result from complex interactions of psychosocial, environmental and genetic factors. While pain may not register as a traditional disease like heart disease or diabetes, the same constellation of factors are at play. The painful experiences throughout our lifetime occur against a background of genes that make us more or less sensitive to pain. But our mental and physical state, previous experiences – painful, traumatic – and the environment can modulate our responses.
If we can better understand what makes individuals more or less sensitive to pain in all kinds of situations, then we are that much closer to reducing human suffering by developing targeted personalized pain treatments with lower risks of misuse, tolerance and abuse than the current treatments. Ultimately, this would mean knowing who is going to have more pain or need more pain-killing drugs, and then being able to effectively manage that pain so the patient is more comfortable and has a quicker recovery.
Not all pain genes are the same
The level of pain an individual senses, mild to excruciating, depends on the types of pain associated genes. donskarpo / Shutterstock.com
With the sequencing of the human genome, we know a lot about the number and location of genes that make up our DNA code. Millions of small variations within those genes have also been identified, some that have known effects and some that don’t.
These variations can come in a number of forms, but the most common variation is the single nucleotide polymorphism – SNP, pronounced “snip” – representing a single difference in the individual units that make up DNA.
There are approximately 10 million known SNPs in the human genome; an individual’s combination of SNPs makes up his or her personal DNA code and differentiates it from that of others. When a SNP is common, it is referred to as a variant; when a SNP is rare, found in less than 1 percent of the population, then it is called a mutation. Rapidly expanding evidence implicates dozens of genes and variants in determining our pain sensitivity, how well analgesics – like opioids – reduce our pain and even our risk for developing chronic pain.
A history of pain tolerance
The first studies of “pain genetics” were of families with an extremely rare condition characterized by the absence of pain. The first report of congenital insensitivity to pain described “pure analgesia” in a performer working in a traveling show as “The Human Pincushion.” In the 1960s there were reports of genetically related families with children who were pain-tolerant.
At that time the technology did not exist to determine the cause of this disorder, but from these rare families we know that CIP – now known by wonkier names like Channelopathy-associated insensitivity to pain and Hereditary Sensory and Autonomic Neuropathy – is the result of specific mutations or deletions within single genes required for transmitting pain signals.
The most common culprit is one of a small number of SNPs within SCN9A, a gene that encodes a protein channel necessary for sending pain signals. This condition is rare; only a handful of cases have been documented in the United States. While it might seem like a blessing to live without pain, these families must be always on alert for severe injuries or fatal illnesses. Typically children fall down and cry, but, in this case, there’s no pain to differentiate between a scraped knee and a broken knee cap. Pain insensitivity means that there is no chest pain signaling a heart attack and no lower right abdominal pain hinting at appendicitis, so these can kill before anyone knows that there is something wrong.
Supersensitivity to pain
Variations within SCN9A not only cause pain insensitivity, but have also been shown to trigger two severe conditions characterized by extreme pain: primary erythermalgia and paroxysmal extreme pain disorder. In these cases, the mutations within SCN9A cause more pain signals than normal.
These types of heritable pain conditions are extremely rare and, arguably, these studies of profound genetic variations reveal little about more subtle variations that may contribute to individual differences in the normal population.
However, with the growing public acceptance of genome-based medicine and calls for more precise personalized health care strategies, researchers are translating these findings into personalized pain treatment protocols that match a patient’s genes.
Many of the answers to why pain sensitivity differs from person to person lies in our genes. Sergei Drozd / Shutterstock.com
Do genetic variations affect pain in everyone?
We know some of the major genes that influence pain perception and new genes are being identified all the time.
We know some of the major genes that influence pain perception and new genes are being identified all the time.
The SCN9A gene is a major player in controlling the body’s response to pain by activating or silencing the sodium channel. But whether it amplifies or dampens pain depends on the mutation an individual carries.
Estimates suggest that up to 60 percent of the variability in pain is the result of inherited – that is, genetic – factors. Stated simply, this means that pain sensitivity runs in families through normal genetic inheritance, much like height, hair color or skin tone.
New painkillers from sea creatures
Therapeutically, we have been using local anesthetics, including lidocaine, to treat pain by inducing a short term block of the channel to stop pain transmission. These drugs have been continuously used to safely and effectively block pain for more than a century.
Interestingly, researchers are evaluating tetrodotoxin, a potent neurotoxin produced by sea creatures like pufferfish and octopuses, which works by blocking pain signal transmission, as a potential pain killer. They have shown early efficacy in treating cancer pain and migraine. These drugs and toxins induce the same state that is present in those with congenital insensitivity to pain.
If there’s one silver lining to the opioid crisis, it is the realization that we need more precise tools to treat pain – ones that treat pain at the source and come with fewer side effects and risk. By understanding the genetic contribution to pain sensitivity, susceptibility to chronic pain and even analgesic response, we can then design treatments that address the “why” of pain and not just the “”where.” We’re beginning to design precision pain management strategies already, and the benefit to humankind will only increase as we know more about why pain differs among people.