21.A way around opioids: Target the type of pain for better pain relief
Three broad categories of pain
Broadly speaking, the medical community now knows there are three types of pain: nociceptive pain, neuropathic pain and inflammatory pain.
Nociceptive pain is experienced when pain receptors, called nociceptors, are activated. For example, go ahead and pinch your skin right now. The pain happens because pressure receptors are being activated on nerves, and pain signals travel quickly to your brain. Some pain nerves have these special receptors, and others have bare nerve endings that can be activated by pressure, stretch, extreme temperature, chemicals or movement. The activated nerve endings send pain signals to the spinal cord and up to the brain. Nociceptive pain is a normal response to insult or injury because it tells the person to protect themselves from further injury.
Nociceptive pain can be divided into two types – somatic, with receptors that monitor the musculoskeletal system, or visceral, with receptors that exist in the lining of intestines. Somatic nociceptive pain results from a broken arm, for example. If a person holds really still and doesn’t move the arm, the pain is not intense. But if a person moves, all the somatic nerve receptors in the bone and muscle are activated and pain is severe. A stomach ulcer is an example of visceral pain. If the stomach and intestines are quiet, there may be little or no pain, but as soon as the stomach and intestines start moving, the pain receptors around the ulcer are activated and severe sharp, burning pain is felt.
Neuropathic pain is felt when nerve fibers are damaged or malfunctioning. A classic example is diabetic peripheral neuropathy, where patients with diabetes feel like pins and needles are stabbing them in their fingers and toes. That is because nerves have been damaged by high levels of sugar. Think of it like a fallen electric power line that has lost its insulation and is now sparking and zapping randomly on the ground. Those random zaps are injured nerves spontaneously firing and sending false signals to the brain that there is something causing pain. Neuropathic pain is pathologic pain, which means that it is considered abnormal. It is not a protective response, as is nociceptive pain; it is a malfunction.
Inflammatory pain is caused by inflammation, the body’s response to injury or infection. In inflammatory diseases, such as infection, traumatic injury, burns, cuts, arthritis, inflammatory bowel disease or autoimmune diseases, the region around the nerve is inflamed. There, an inflammatory soup of pain signal molecules, such as TGN-alpha, IL-1, IL-6 and ATP, lower the threshold for nerve firing, so even the slightest thing sets them off. Inflammation causes nerves to signal pain much easier than they otherwise would.
22.What is chronic pain and why is it hard to treat?
A recent study by the National Institutes of Health (Estimates of Pain Prevalence and Severity in Adults: United States, 2012) found that more than one in three people in the United States have experienced pain of some sort in the previous three months. Of these, approximately 50 million suffer from chronic or severe pain.
Pain can have a purpose
I study the processes that trigger and maintain chronic pain. One of the first things I teach my students is that pain is a biological process that is critical for life. Pain protects our bodies from injury and by reminding us that tissue is damaged and needs to be protected it also aids in repairing the injuries we do acquire.
What concerns those of us who treat and study pain, however, is chronic pain. This type of pain – that can last for weeks, months or even years – serves no useful purpose for survival and is actually detrimental to our health.
How do we experience pain?
The human pain experience can be divided into three dimensions: what pain researchers call the sensory-discriminative, the affective-motivational and the cognitive-evaluative. In acute pain there is a balance between each of these dimensions that allows us to accurately evaluate the pain and the threat it may pose to our survival. In chronic pain these dimensions are disrupted.
The sensory-discriminative dimension refers to the actual detection, location and intensity of the pain. This dimension is the result of a direct nerve pathway from the body to the spinal cord and up into the brain’s cortex. This is how we are aware of the location on our bodies of a potential injury and how much damage may be associated with the injury.
Knowing where it hurts is only part of experiencing pain. Is your injury life-threatening? Do you need to run away or fight back? This is where the affective-emotional dimension comes in. It arises from the pain circuitry interacting with the limbic system (the emotional centers of the brain). This adds an emotional flavor to the incoming pain signal and is part of the fight-or-flight response. This pathway evokes the anger or fear associated with the possibility of physical harm. It also provokes learning so that in the future we avoid the circumstances leading to the injury.
The third dimension, the cognitive-evaluative, is the conscious interpretation of the pain signal, combined with other sensory information. This dimension draws on the different aspects of pain processing allowing us to determine the location and potential severity of an injury and to come up with survival strategies based on all available information.
23.Why it’s so hard for doctors to understand your pain
We’re all human beings, but we’re not all alike. Each person experiences pain differently, from an emotional perspective as well as a physical one, and responds to pain differently.
Today, however, doctors are under pressure to limit costs and prescribe treatments based on standardized guidelines. A major gap looms between the patient’s experience of pain and the limited “one size fits all” treatment that doctors may offer.
The hope of genetic research
My guess is that the next decades will bring an explosion in research illuminating the genetic mechanisms behind pain experiences. Genetic differences can help explain why some patients develop certain diseases while others, exposed to the same environmental factors, never do. Some patients undoubtedly are more sensitive to pain from the start than others, based on genetic factors that the medical community doesn’t yet understand.
At UCLA, where I work, the Institute for Precision Health obtains a sample of blood from nearly every surgical patient. By analyzing each patient’s genetic data, we hope to explain why patients often respond so differently after the same type of surgery, injury or illness.
Furthermore, chronic pain is associated with long-lasting changes in gene expression in the central nervous system. Simply put, the experience of pain changes a patient’s nervous system at the molecular level. These changes are linked to behavioral expressions of pain. Emotional factors – including a history of previous traumatic stress or depression – increase the chances that a patient will become dependent on opioids after experiencing pain.
24.Explainer: what is pain and what is happening when we feel it
Pain doesn’t originate at the site as most think, it’s created by the brain so we protect the area that’s in danger. Pain scientists are reasonably agreed that pain is an unpleasant feeling in our body that makes us want to stop and change our behaviour. We no longer think of pain as a measure of tissue damage – it doesn’t actually work that way even in highly controlled experiments. We now think of pain as a complex and highly sophisticated protective mechanism.
How does pain work?
Our body contains specialised nerves that detect potentially dangerous changes in temperature, chemical balance or pressure. These “danger detectors” (or “nociceptors”) send alerts to the brain, but they cannot send pain to the brain because all pain is made by the brain.
Pain is not actually coming from the wrist you broke, or the ankle you sprained. Pain is the result of the brain evaluating information, including danger data from the danger detection system, cognitive data such as expectations, previous exposure, cultural and social norms and beliefs, and other sensory data such as what you see, hear and otherwise sense.
The brain produces pain. Where in the body the brain produces the pain is a “best guess scenario”, based on all the incoming data and stored information. Usually the brain gets it right, but sometimes it doesn’t. An example is referred pain in your leg when it is your back that might need the protecting.
It is pain that tells us not to do things – for example, not to lift with an injured hand, or not to walk with an injured foot. It is pain, too, that tells us to do things – see a physio, visit a GP, sit still and rest.
We now know that pain can be “turned on” or “turned up” by anything that provides the brain with credible evidence that the body is in danger and needs protecting.
All in your head?
So is pain all about the brain and not at all about the body? No, these “danger detectors” are distributed across almost all of our body tissues and act as the eyes of the brain.
When there is a sudden change in tissue environment – for example, it heats up, gets acidic (cyclists, imagine the lactic acid burn at the end of a sprint), is squashed, squeezed, pulled or pinched – these danger detectors are our first line of defence.
They alert the brain and mobilise inflammatory mechanisms that increase blood flow and cause the release of healing molecules from nearby tissue, thus triggering the repair process.
Local anaesthetic renders these danger detectors useless, so danger messages are not triggered. As such, we can be pain-free despite major tissue trauma, such as being cut into for an operation.
Inflammation, on the other hand, renders these danger detectors more sensitive, so they respond to situations that are not actually dangerous. For example, when you move an inflamed joint, it hurts a long way before the tissues of the joint are actually stressed.
Danger messages travel to the brain and are highly processed along the way, with the brain itself taking part in the processing. The danger transmission neurones that run up the spinal cord to the brain are under real-time control from the brain, increasing and decreasing their sensitivity according to what the brain suggests would be helpful.
So, if the brain’s evaluation of all available information leads it to conclude that things are truly dangerous, then the danger transmission system becomes more sensitive (called descending facilitation). If the brain concludes things are not truly dangerous, then the danger transmission system becomes less sensitive (called descending inhibition).
25.Pain really is in the mind, but not in the way you think
What is pain?
The International Association for the Study of Pain defines pain as an experience. Pain is usually triggered by messages that are sent from the tissues of the body when those tissues are presented with something potentially dangerous.
The neurones that carry those messages are called nociceptors, or danger receptors. We call the system that detects and transmits noxious events “nociception”. Critically, nociception is neither sufficient nor necessary for pain. But most of the time, pain is associated with some nociception.
The exact amount or type of pain depends on many things. One way to understand this is to consider that once a danger message arrives at the brain, it has to answer a very important question: “How dangerous is this really?” In order to respond, the brain draws on every piece of credible information – previous exposure, cultural influences, knowledge, other sensory cues – the list is endless.
26.The 2021 Nobel Prize for medicine helps unravel mysteries about how the body senses temperature and pressure
Humans rely on our senses to tell us about the world. Which way is that waterfall? Is it day or night? Is that food fresh or spoiled?
Such questions are harder to answer if our sensory systems can’t detect the sound of rushing water, the shimmer of moonlight or the odor of spoiled milk. Prior to this week, the Nobel Committee for Physiology or Medicine had recognized important advances in our understanding of how sensations are detected in three sensory systems: hearing, vision and smell.
Now, the Nobel Committee has awarded this year’s prize in medicine to two scientists who have advanced our understanding of this detection process for “somatosensation,” the sense responsible for the perceptions of touch, temperature, vibration, pain and proprioception – the body’s ability to sense its own movements and position in space.
…… were awarded the Nobel Prize in Physiology or Medicine for their pioneering work identifying proteins that the body uses to detect temperature and pressure. These two scientists led teams that unraveled key steps in the processes by which temperature and pressure are recognized by sensory cells and converted into signals that can be interpreted by the brain as perceptions such as warmth, cold or texture.
The work of Julius and Patapoutian has greatly expanded scientists’ views of how the nervous system deciphers the external and internal world by introducing us to entirely new classes of sensory receptors. Their findings have yielded critical and novel insights into the physiology of temperature, pain and touch sensation.
Bringing the heat
Nociceptors are special sensory neurons that carry pain information, including pain from potentially damaging levels of heat. Scientists who study pain had known for years that capsaicin – the chemical in chiles responsible for their perceived heat – activates nociceptors.
To do this, they tested thousands of different proteins produced by rodent sensory neurons until they found one that responded to capsaicin and its chemical cousins. As predicted, this protein also responded to high temperatures, indicating that it was the long sought-after heat sensor in these neurons.
This protein, named TRPV1, was the first of a group of related proteins discovered by Julius’ lab and other groups that respond to diverse plant chemicals and different temperatures. For example, the protein TRPM8 is activated by both cold and menthol, the chemical that causes the cooling sensation of mint, while the protein TRPA1 is turned on by the pungent compounds found in garlic.
Finding the touch
They took a clever approach. Instead of testing the products of single genes for their ability to respond to pressure – a strategy that worked so well for identifying the capsaicin receptor – Patapoutian and his team instead silenced single genes, one by one, in a touch-sensitive cell until the cell lost its ability to respond.
They then confirmed in nerve cells that two related proteins, named Piezo1 and Piezo2, mediated responses to physical stimulation. Later, the Patapoutian group and others showed more directly that Piezo proteins are critical for touch itself.
Opening doors to new scientific discoveries
The discoveries of Julius and Patapoutian have given sensory researchers fundamental insights into how people interact with their world. But they will almost certainly lead to important medical advances as well.
For example, red blood cells also express Piezo1, which may help them change shape to fit through tiny capillaries. However, certain mutations in Piezo1 can lead to deformed red blood cells and a rare type of anemia, in which red blood cell numbers are depleted.
Topical capsaicin creams are already used by many people as over-the-counter treatments for the relief of minor muscle pains. But this family of temperature-sensing proteins could also prove to be useful targets for new drugs aimed at treating debilitating, chronic pain.
Nature gave us a hint that a whole new world of biology was waiting to be discovered. Julius and Patapoutian have now pointed the way.
27.去极化(depolarization)和动作电位(action potential)
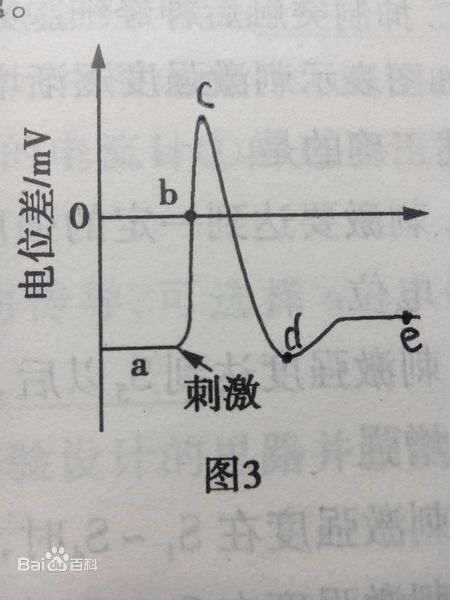
去极化(depolarization)又称除极化,是指将膜极化状态变小的变化趋势或者静息电位向膜内负值减小的方向变化。如右图所示,去极化为ab阶段。去极化是通过向膜外的电流流动或改变外液的离子成分而产生的。
一般细胞的内部以细胞膜为界,内部具负电性,这种极性程度的减弱称为去极化。与此相反,其增强的,则称为超极化。去极化是通过向膜外的电流流动或改变外液的离子成分而产生的。对兴奋性膜使其在一定阈值以下去极化,则产生主动的去极化,也常产生极化方向的逆转(overshoot),但以后通过复极化(repolarization)而返回原来电位,称此为动作电位。神经细胞兴奋时将产生去极化,细胞兴奋产生的电位变化即为动作电位(action potential)。
脑内细胞膜的稳定,会协调神经传递功能的正常,反应敏锐,神经的传递与反馈,除了传出神经系统递质外,还依存于电压依赖性的离子通道。抗癫痫药主要是阻断电压依赖性离子通道发挥作用。
脑内细胞膜去极化效应,会对脑内思维活动与外周神经的肢体运动,疼痛感觉等产生变化。这种作用的产生,有药物直接对细胞膜离子通道发生作用,也有是兴奋与抑制反馈产生耐受性调整。影响的因素很多,涉及能够影响神经运动与感觉的药物都会对其产生作用,可以说是神经特有的细胞功能,平衡稳定机体的协调。
阻断降低电压依赖性离子通道,会产生脑内细胞膜去极化阈值升高,使神经不容易兴奋,尤其是痛觉抑制最明显。有效的降低神经的活动强度,使人处于相对安静状态,对一些疾病症状的感觉也不明显,有时会感到舒服轻松的感觉。可实际对人影响还是很大,情绪会一直处于低落,兴趣感会下降,思维能力强度也会被抑制,长期会产生抑郁的情绪。
动作电位(action potential)是指可兴奋细胞受到刺激时在静息电位的基础上产生的可扩布的电位变化过程。动作电位由峰电位(迅速去极化上升支和迅速复极化下降支的总称)和后电位(缓慢的电位变化,包括负后电位和正后电位)组成。峰电位是动作电位的主要组成成分,因此通常意义的动作电位主要指峰电位。动作电位的幅度约为90~130mV,动作电位超过零电位水平约35mV,这一段称为超射。神经纤维的动作电位一般历时约0.5~2.0ms,可沿膜传播,又称神经冲动,即兴奋和神经冲动是动作电位意义相同。
28.疼痛遗传学的研究方法
【疼痛遗传学研究的两个分支】
-
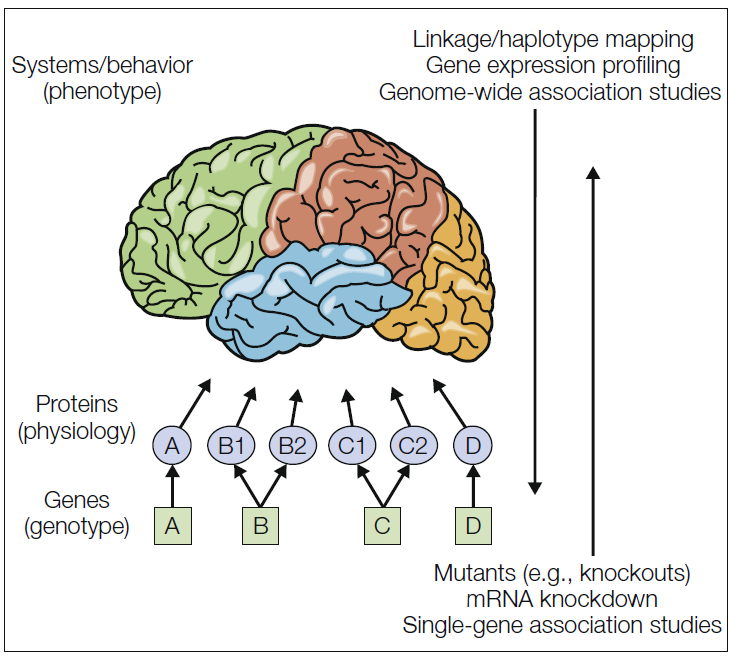
One type of pain genetics asks the question, which genes are relevant to pain?
-
The second type of pain genetics asks the question, of the pain-relevant genes, which are responsible for individual differences in sensitivity to pain and analgesia and for differential susceptibility and/or expression of painful pathologies?
【回答上述问题的两种策略】
-
“Bottom-up” (genotype → phenotype)
-
“Top-down” (phenotype → genotype)
With a top-down strategy, one examines populations showing constrasting systems-level phenotypes and tries to find the genes responsible for the differences.
29.What is the difference between pain threshold and pain tolerance?
Pain threshold refers to the lowest intensity at which a given stimulus is perceived as painful; it is relatively constant across subjects for a given stimulus. For example, most subjects will define a thermal stimulus as painful when it reaches about 50° C. Similarly, barring disease states, mechanical pressure produces pain at approximately the same amount of pressure across subjects. Pain threshold as it relates to sensitivity to pressure is measured with an algometer.
Pain tolerance, on the other hand, is the greatest level of pain that a subject is prepared to endure. Tolerance varies much more widely across subjects and depends on prescribed medications. Clinically, pain tolerance is of much more importance than pain threshold. (More detailed discussions of threshold and tolerance are found in Chapter 6, Pain Measurement.)
30.Reflections on Pain Sensitivity
这篇关于pain sensitivity的文章写得很好,可以用于汇报时候的Introduction。
Pain sensitivity is thought to be a characteristic of each individual that affects the way a painful stimulus is perceived. In simple terms, being pain hyper- or hyposensitive results in the perception of the same stimulus as very painful or slightly painful, respectively. As a matter of fact, the same trauma results in extremely different amounts of pain reported by different individuals: extensive tissue damage is not always associated with uncontrollable pain, and minor tissue damage may be associated with excruciating pain. Therefore, something beyond tissue damage must play a role in pain perception. This “something” is frequently identified as individual pain sensitivity.